Vasectomy is a surgical procedure primarily aimed at male contraception by preventing the passage of sperm into the semen. This procedure is often seen as a permanent form of birth control for men who are certain that they do not want to have children in the future. However, as with any medical procedure, there are a number of factors to consider when it comes to its effect on male fertility. In this comprehensive analysis, we will explore the procedure of vasectomy, its impact on male fertility, potential reversibility, and the broader implications for men’s health.
1. Understanding Vasectomy
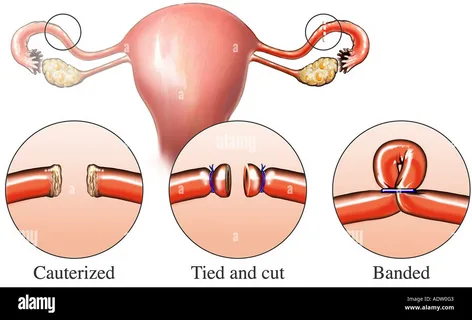
A vasectomy involves the cutting or blocking of the vas deferens, which are the tubes responsible for carrying sperm from the testicles to the urethra. When these tubes are disrupted, sperm are prevented from mixing with semen during ejaculation, effectively rendering a man sterile. The procedure is typically performed under local anesthesia and takes about 15 to 30 minutes to complete. It is considered a highly effective form of contraception, with a failure rate of less than 1%.
There are two main types of vasectomy procedures: the conventional vasectomy and the no-scalpel vasectomy. Both aim to achieve the same result, though the no-scalpel procedure is generally less invasive and requires a smaller incision, leading to fewer complications and a quicker recovery time.
2. Vasectomy and Male Fertility
Before undergoing a vasectomy, many men are concerned about its long-term effects on male fertility. While a vasectomy effectively prevents pregnancy by stopping the release of sperm, the procedure does not impact the production of sperm in the testicles. Men who undergo a vasectomy will still produce sperm, but it will be absorbed by the body rather than being released during ejaculation.
3. How Vasectomy Affects Sperm Production
The procedure doesn’t interfere with the production of sperm, which continues in the testes after a vasectomy. The main effect of the vasectomy is the obstruction of sperm from reaching the urethra, where it would otherwise mix with semen. As a result, sperm is reabsorbed by the body. This process is natural and does not have any significant impact on a man’s overall health. However, since the sperm can no longer exit the body through ejaculation, men who have undergone the procedure will be sterile.
It is important to note that even though sperm are still produced, they are not viable for fertilization unless the vasectomy is reversed or other assisted reproductive techniques are employed. The absence of sperm in the semen is what makes the procedure effective as a form of birth control.
4. Long-Term Effects on Male Fertility
In most cases, vasectomy is seen as a permanent procedure. However, there are instances where men may later decide they want to reverse the procedure and regain their fertility. There are two types of vasectomy reversal procedures: vasovasostomy and vasoepididymostomy. These procedures aim to reconnect the vas deferens or bypass any blockages in the male reproductive tract, allowing sperm to once again enter the semen. The success of these procedures depends on various factors, such as the time elapsed since the original vasectomy, the age of the man, and the technique used for reversal.
5. Vasectomy Reversal: Is It Effective?
Vasectomy reversal is possible, but it is not guaranteed to restore fertility. The chances of success depend on the length of time since the original vasectomy and the method used for the procedure. Generally, the earlier the reversal is performed after a vasectomy, the higher the likelihood of success. If the procedure is performed within 10 years of the original vasectomy, success rates may be as high as 90%. However, if more than 10 years have passed, the success rate tends to decrease, often falling to around 50-60%.
The two methods of vasectomy reversal, vasovasostomy and vasoepididymostomy, have varying degrees of success. The former is used when the vas deferens can be reconnected directly, while the latter is used when there are blockages in the epididymis (a tube that connects the testicle to the vas deferens). A skilled surgeon will evaluate the man’s reproductive anatomy and choose the most appropriate method for the reversal.
It is also important to note that even if a vasectomy reversal is successful and sperm is present in the semen, it does not guarantee the ability to conceive. Many men may still face difficulties with infertility due to other factors, such as sperm quality, sperm count, or female infertility issues.
6. Alternative Options for Fatherhood After Vasectomy
For men who undergo a vasectomy but later decide they want children, there are a number of fertility options available. These include:
- Sperm Retrieval and In Vitro Fertilization (IVF): Even if a vasectomy is performed, sperm can still be retrieved directly from the testicles or epididymis through a surgical procedure. The retrieved sperm can then be used in an in vitro fertilization (IVF) process, where the sperm is combined with an egg in a laboratory setting to create an embryo. This method is often used for men who have had a vasectomy and want to pursue biological fatherhood.
- Donor Sperm: In cases where a vasectomy reversal is not successful or not feasible, men may also consider using donor sperm to father a child. This option is commonly used in conjunction with IVF, where a woman may be inseminated with sperm from a donor, bypassing the need for the man’s sperm.
- Adoption: For those who no longer wish to pursue biological parenthood, adoption is always an option. This is an increasingly popular choice for men and women who wish to become parents but face fertility challenges.
7. Psychological and Emotional Considerations
While vasectomy is typically considered a permanent form of contraception, the decision to undergo the procedure is often not made lightly. Many men experience psychological challenges after the procedure, especially if they are later confronted with the possibility of wanting children. Feelings of regret, anxiety, and uncertainty are common, particularly if the man’s partner is unable to conceive or if their life circumstances change.
It is important to approach the decision of having a vasectomy with careful consideration and communication between partners. Men should be certain of their decision to avoid future emotional distress. Counseling and support groups may also be helpful in providing guidance and reassurance for men considering this life-changing procedure.
8. Health Considerations and Complications
While vasectomy is generally considered a safe and straightforward procedure, there are some risks and potential complications associated with it. These include:
- Infection: As with any surgical procedure, there is a risk of infection at the site of the incision or within the reproductive tract.
- Hemorrhage: Bleeding during or after the procedure can lead to swelling or hematoma (a collection of blood under the skin).
- Post-Vasectomy Pain Syndrome: Some men experience chronic pain or discomfort in the testicles or scrotum after a vasectomy. This condition can persist for months or even years and may require additional treatment.
- Sperm Granuloma: This is a condition where sperm leaks into the tissue and forms a small, hard lump. It can cause pain and may need to be treated surgically in some cases.
Despite these risks, the complications associated with vasectomy are rare, and most men experience no significant long-term side effects.
9. The Role of Vasectomy in Family Planning
Vasectomy plays a critical role in modern family planning. For many men and their partners, it is an effective and permanent solution to prevent unwanted pregnancies. It allows couples to take control of their reproductive choices and avoid the need for other forms of contraception, such as condoms or hormonal methods. While the procedure is permanent, it is an option that can be reconsidered in the future with the help of a reversal procedure or assisted reproductive techniques.
As society continues to evolve, vasectomy is becoming an increasingly popular option for men who have completed their families and are certain they do not wish to have any more children. The high success rate and minimal complications make it a reliable choice, and as our understanding of male fertility improves, it is likely that new techniques and treatments will emerge to further refine the procedure and its outcomes.
Conclusion
In conclusion, a vasectomy is a highly effective form of contraception with minimal risks. It provides men with a permanent means of birth control, and while it may impact male fertility by preventing sperm from reaching the semen, it does not affect sperm production. Although a vasectomy is intended to be permanent, there are options available for men who later wish to have children, including vasectomy reversal, sperm retrieval, and IVF. It is important to approach the decision to undergo a vasectomy with careful consideration, as it can have psychological and emotional impacts. Overall, vasectomy remains a significant choice in family planning and male fertility management, offering men control over their reproductive health.