In today’s rapidly evolving healthcare landscape, ophthalmology practices face increasing pressure to balance exceptional patient care with effective financial management. From cataract surgeries to glaucoma treatments, ophthalmologists provide essential services but without a streamlined Revenue Cycle Management (RCM) system in place, even the most skilled practice can experience financial strain.
This post explores the unique challenges and solutions involved in ophthalmology RCM, and why outsourcing to specialized partners like GlobalV can transform a practice’s performance.
What is Revenue Cycle Management in Ophthalmology?
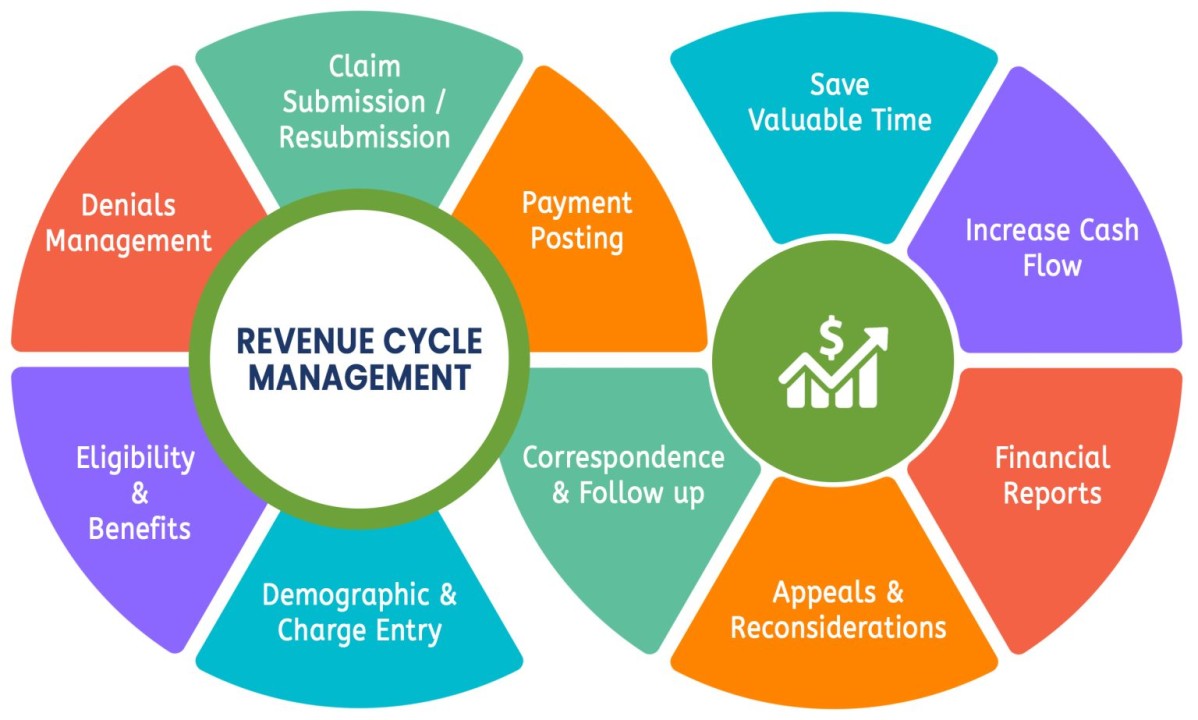
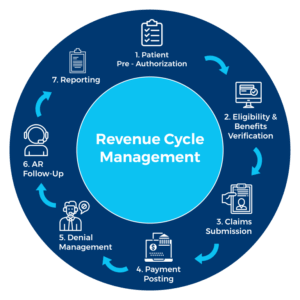
Revenue Cycle Management refers to the financial process healthcare providers use to track patient care episodes from initial appointment scheduling to the final payment. In ophthalmology, this cycle includes a range of specialized services, from routine exams to complex surgical procedures, which must be correctly documented, coded, billed, and reimbursed.
The RCM process includes:
-
Patient scheduling and eligibility verification
-
Accurate charge capture
-
Proper CPT/ICD-10 coding
-
Claims submission
-
Denial management
-
Patient billing and collections
-
Revenue reporting and analytics
Unlike primary care or general specialties, ophthalmology requires a deep understanding of nuanced coding, payer rules, and compliance requirements.
Looking to improve patient communication and front-desk efficiency? Explore our Call Handling Review services to enhance call quality and staff performance.
Challenges Unique to Ophthalmology RCM
1. Complex Coding Structures
Ophthalmology procedures often involve unique CPT codes and modifiers that vary based on diagnosis, location, and laterality (right or left eye). Improper use can lead to denied or underpaid claims.
2. Multiple Payer Rules
Medicare and private insurers often have different coverage criteria for vision-related vs. medical eye care. Navigating these payer-specific rules requires experience and precision.
3. Pre-authorization Requirements
Certain procedures, such as intravitreal injections or refractive surgeries, require prior authorization. Missing this step can result in claim rejection and revenue loss.
4. Patient Responsibility
As high-deductible plans become more common, patients are responsible for a greater portion of their care costs. This shift increases the importance of effective patient communication and collection strategies.
5. Denial Management
Denied claims due to missing information, incorrect codes, or untimely submissions can delay cash flow. A lack of structured follow-up processes compounds the problem.

The Cost of Inefficient RCM
An inefficient RCM system doesn’t just delay revenue—it directly impacts the financial sustainability of the practice. Some of the tangible consequences include:
-
Increased accounts receivable (A/R) days
-
Higher claim denial rates
-
Lower collection rates
-
Rising overhead due to administrative burdens
-
Loss of patient trust due to billing confusion
With ophthalmology practices managing high patient volumes and sophisticated treatments, these inefficiencies can quickly lead to burnout, frustrated staff, and stagnant growth.
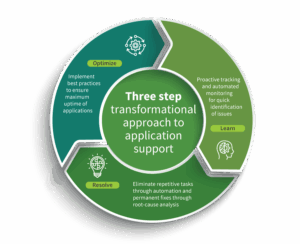
Strategic RCM Solutions for Ophthalmology Practices
To overcome these challenges, ophthalmology practices need more than a basic billing system. They need a comprehensive, end-to-end RCM solution tailored to the specialty.
1. Ophthalmology-Specific Coding Expertise
Hiring or partnering with certified coders who understand the intricacies of ophthalmology coding (e.g., modifier usage, bilateral procedures, bundled services) is critical.
2. Automated Eligibility Checks
Before a patient steps into the exam room, real-time verification of benefits ensures correct coverage, reducing denials related to eligibility or plan exclusions.
3. Prior Authorization Management
Using systems or services that manage authorizations helps ensure approval is obtained before procedures are performed.
4. Real-Time Claims Scrubbing
Automated scrubbing tools review claims for errors before submission, minimizing the risk of denials or payer rejections.
5. Denial Analytics and Resolution
Identifying denial trends and establishing workflows to appeal or correct rejected claims improves the first-pass resolution rate and boosts cash flow.
6. Patient-Friendly Billing
Providing patients with clear statements, digital payment options, and support improves collection rates and satisfaction.
7. Revenue Insights and Reporting
Monitoring KPIs such as days in A/R, clean claim rate, and patient collections provides valuable insights into operational efficiency and helps guide future decisions.
Why Partnering with an RCM Provider Like GlobalV Makes Sense
Managing all these components in-house is time-consuming and requires specialized knowledge. Many successful ophthalmology practices are turning to RCM service providers to handle these operations more efficiently.
GlobalV’s Ophthalmology-Focused RCM Services Include:
Medical Coding & Billing
Certified ophthalmology coders ensure every visit, test, and procedure is accurately coded to maximize reimbursement.
Claims Submission & Denial Management
From clean claim submission to prompt denial follow-up, GlobalV ensures steady cash flow and reduced claim rework.
Prior Authorization Support
Streamlined systems and trained staff handle pre-authorizations, removing administrative burdens from clinical teams.
Patient Billing & Collections
Clear, timely patient statements and professional call center support lead to faster collections and better patient experiences.
Performance Reporting
GlobalV delivers real-time insights and custom reports, empowering practices to make data-driven decisions and stay ahead.
Credentialing Services
GlobalV ensures your providers are properly credentialed with all payers, a critical factor in avoiding reimbursement delays.
Key Benefits of Outsourcing Ophthalmology RCM
Whether you’re a solo ophthalmologist or part of a growing eye care group, outsourcing RCM to a specialized provider like GlobalV offers measurable benefits:
-
Reduced Claim Denials
-
Shorter A/R Cycles
-
Increased Revenue Collection
-
Lower Administrative Costs
-
Improved Compliance
-
Enhanced Patient Satisfaction
-
Scalable Systems to Support Growth
By delegating the financial side of the practice to experts, ophthalmologists can refocus on what they do best—delivering top-tier patient care.
Conclusion: The Future of Financial Health in Ophthalmology
In a specialty where precision is everything, ophthalmology practices must apply the same attention to detail in their revenue cycle as they do in the exam room. By implementing tailored RCM strategies—or better yet, partnering with a specialized provider like GlobalV—eye care professionals can secure a more predictable and profitable financial future.
Whether you’re facing growing claim denials, overwhelmed billing staff, or simply looking to improve operational efficiency, embracing ophthalmology-focused RCM is a smart investment in your practice’s success.